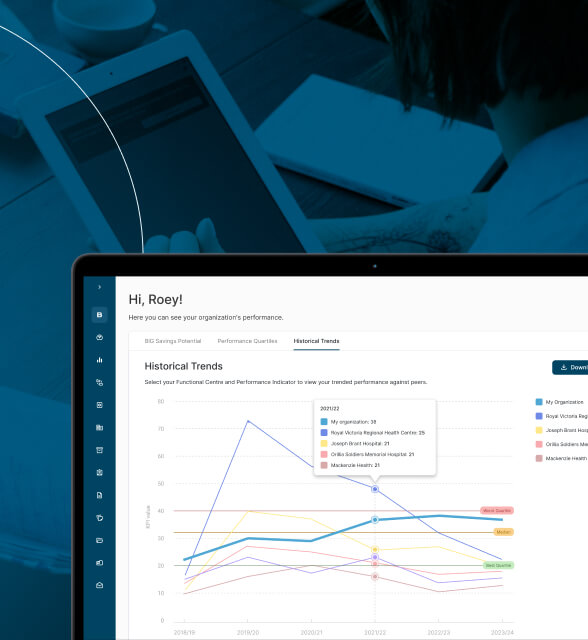
End-to-End RCM Automation
Platform
Business need
GoodBilling set out to eliminate one of the biggest sources of friction in revenue cycle management: uncertainty and manual work across eligibility checks, verification of benefits (VoB), documentation, coding alignment, and claim creation. Their goal was to build a system that could scale to hundreds of thousands of claims per month while keeping human oversight to a minimum.
Result
MindK partnered with GoodBilling to design and build a solution that automates the entire flow from patient intake and benefits verification to EMR integration and claim generation. A team of 10 specialists across engineering, project management, data engineering, and DevOps delivered the first production version in 5 months, while meeting strict healthcare security and privacy requirements.
Want to learn how MindK can automate your RCM processes with our AI agents? Request a free no-obligation consultation →
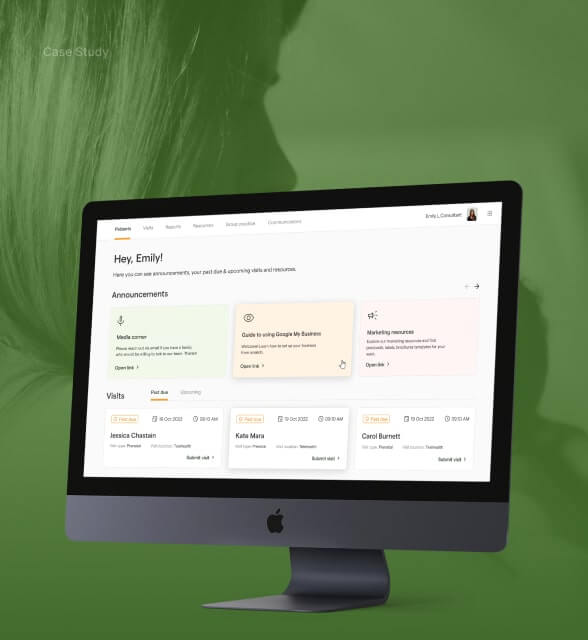
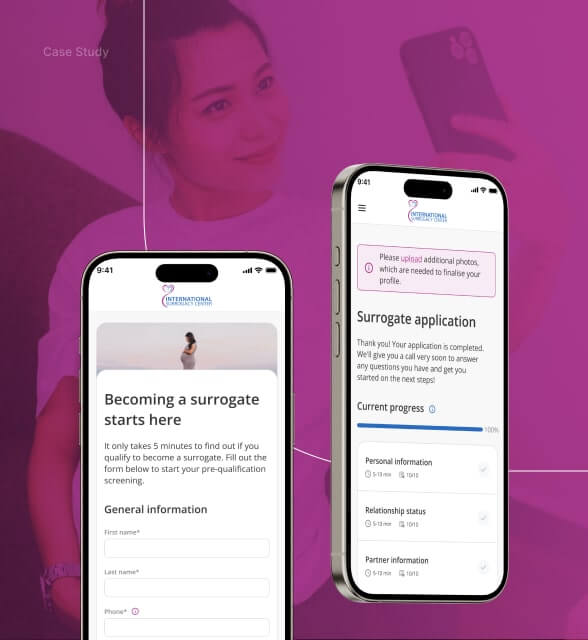
Easy patient onboarding with an embedded link
Upfront out of pocket cost estimation
Intelligent Benefits Verification
Matching of patient context to payable codes
Bidirectional integration with major EMR systems
Webhooks Triggered by Signed Clinical Notes
Anonymizer service for HIPAA compliant AI processing
In-Environment Model Hosting for Sensitive Tasks
Payer Portal AI Agents
Voice Agents That Navigate IVR and Talk to Payer Support
The voice agent is essential for payers and plan types where portal automation isn’t sufficient.
Secure, HIPAA-compliant infrastructure
from day one
MindK implemented a HIPAA-compliant infrastructure using AWS-native services and hardened operational protocols. Key principles included strong security for in transit and at rest, segmented services for PHI vs non-PHI processing, and operational controls designed for healthcare-grade environments.
Tech stack
Business value
1
1
1
Work with RCM experts
Let us know about your technology challenges and we'll
help you resolve them.